The Problem
17 Veterans kill themselves every day.
6,000 Veterans kill themselves every year. 8
The Veteran suicide rate is 1.5 times greater than that of non-Veterans.9
The suicide rate is highest among 18-34-year-old Veterans— the post 9/11 generation.10
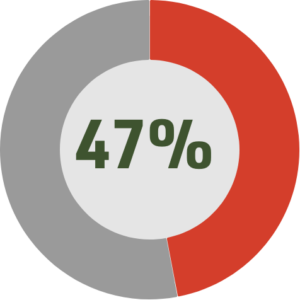
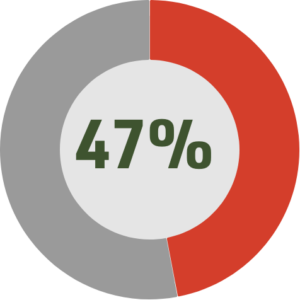
Between 19% and 44% of Veterans returning from Iraq and Afghanistan meet criteria for mental health disorders, such as PTSD or depression. Yet, 47% do not seek mental health support.
Four primary barriers stand in their way:

“As much as they talk about getting help if you need it, they still have this tendency to portray that it’s weakness.”
Personal and Professional Stigma
43.6%
of post-9/11 Veterans fear that seeking mental health support will harm their career.
38%
fear their coworkers would lose respect for them if they sought help.11

“You don’t want to tell your boss that you have an appointment for something behavioral health. You like to hide those problems.”
Lack of Trust
45%
believe their friends and family would be better help than a professional.
29%
fear that their treatment will not be kept confidential.12

“They say I always have appointments and they always want me to bring a note in, bring a note after I’m done.”
Bureaucracy
18 days
is the average wait time for treatment at a VA facility.
125,000
post-9/11 Veterans were discharged at other-than-honorable status, leaving them ineligible for benefits.13

“Every time I called back it was, ‘Oh, call back next week. Call back next week.’ Sometimes one of the big things is just the feeling … that it’s not really their priority to get you.”
Geography
15 miles
The nearest VA facility with mental health services is over 15 miles away from most Veterans.
25%
of American Veterans live in areas designated as rural by the U.S. Census Bureau.14
8Department of Veterans Affairs, Veterans Health Administration. 2018. “VA National Suicide Data Report 2005-2016.” Office of Mental Health and Suicide Prevention. 9 Department of Veterans Affairs, Veterans Health Administration. 2018. “VA National Suicide Data Report 2005-2016.” Office of Mental Health and Suicide Prevention. 10 Department of Veterans Affairs, Veterans Health Administration. 2018. “VA National Suicide Data Report 2005-2016.” Office of Mental Health and Suicide Prevention. 11 Tanielian, T., Jaycox, L., Schell, T., Marshall, G., Burnam, M., Eibner, C., … Vaiana, M. (2008). Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery . RAND Center for Military Health Policy Research. doi: 10.7249/mg720.1 12Tanielian, T., Jaycox, L., Schell, T., Marshall, G., Burnam, M., Eibner, C., … Vaiana, M. (2008). Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery . RAND Center for Military Health Policy Research. doi: 10.7249/mg720.1 13 Audit of Veteran Wait Time Data, Choice Access, and Consult Management in VISN 15. Department of Veteran Affairs Officer of Inspector General. (2018, March 13). https://www.va.gov/oig/pubs/VAOIG-17-00481-117.pdf 14 Holder, Kelly Ann. 2016. “Veterans in Rural America: 2011-2015.” American Community Survey Reports, ACS-36, US Census Bureau. 15Tanielian, T., Jaycox, L., Schell, T., Marshall, G., Burnam, M., Eibner, C., … Vaiana, M. (2008). Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery . RAND Center for Military Health Policy Research. doi: 10.7249/mg720.1


